Concept Schematic
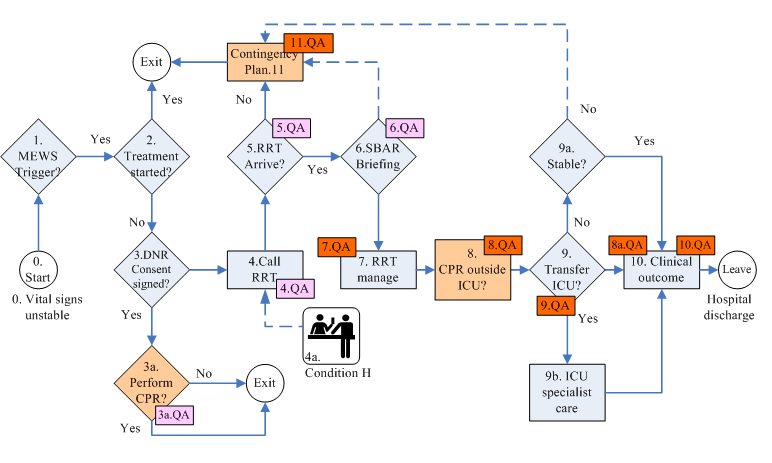
(click on individual parts of map to hyperjump to relevant text section)
Schematic Legend
- Orange background : failure to proceed smoothly, requiring quality improvement efforts.
- Pink background QA : monitor process compliance
- Red background QA : a clinical outcome indicator
Monitoring Effectiveness
-
Total CPR events per 1,000 discharges
- CPR events outside ICU per 1,000 discharges {8.QA}
-
Hospital mortality {10.QA}
- Mortality rate at discharge for CPR patients
- Mortality rate for ward CPR patients {8a.QA}
- Number of unplanned ICU admissions {9.QA}
- Staff satisfaction {7.QA}
Monitoring Process Compliance
- CPR on DNR patients per 1,000 discharges {3a.QA}
- RRT activations per 1,000 discharges {4.QA}
- RRT activations by ward per 1,000 discharges {4.QA}
- Express handover (SBAR) compliance {6.QA}
- Response time compliance {5.QA}
Why not CPR team?
The average survival rate to hospital discharge for all patients undergoing CPR was only 10~15% between 1983~1989, and has not improved measurably since. For patients with certain diagnoses (e.g. metastic cancers), survival rates are even lower.
Furthermore, patients who were successfully resuscitated often undergo aggressive treatment in the intensive care unit and suffer complications including rib fractures, permanent neurological deficits, and impaired functional status. Even without physical injury, CPR can lead to psychological harm that lowers survivors' quality of life.
Failure to Rescue from Complication
Failure to rescue (FTR) refers to a death after a treatable complication. The rate of FTR in surgical patients derived from routine administrative data is recognized as an important indicator of patient safety (in the USA).
Definition of "Rapid Response Team/System"
Afferent arm (the criteria for calling)
- Bedside staff are encouraged to call the team when any of a number of prespecified criteria are met.
- At certain hospitals, patients and family members are also permitted to call the team.
- More sophisticated "track-and-trigger" bedside monitoring systems automatically trigger intervention when certain physiologic abnormalities are detected.
Efferent arm (system response)
A team of clinicians who bring critical care expertise to the patient bedside, outside the ICU.
The team provides an emergency response to stabilise a deteriorating patient until the patient can be cared for by the home team or is transferred to a higher leverl of care. The team does not provide a consultation service and does not take over the care of the patient on the ward.
Despite differences in team structure, the criteria used to summon the teams are generally similar.
Background
Rapid response teams (RRTs) are one of six initiatives that comprised the Institute for Healthcare Improvement's (IHI's) "100,000 Lives Campaign". The idea is that any health care worker can bypass the typical chain of command and call what is essentially a medical "SWAT team" to quickly assess a patient and intervene when lifesaving care may be needed. Unlike the traditional "code" team, the RRT intervenes before the patient experiences respiratory or cardiac arrest.
RRTs may consist of any of the following staff positions:
- Physician – senior resident or intensivist or hospitalist
- Physician's assistant
- Critical care RN
- Clinical nurse specialist
- Respiratory therapist
In every model, there are three key features of the team members:
- They must be available to respond immediately when called, and not be constrained by competing responsibilities.
- They must be onsite and accessible.
- They must have the critical care skills necessary to assess and respond.
3a. DNR
A "do not resuscitate" (DNR) order indicates that a person has decided not to have cardiopulmonary resuscitation (CPR) attempted in the event his or her heart or breathing stops. A DNR order is written by a physician after discussing the burdens and benefits of CPR with the patient or the patient’s surrogate decision maker. A DNR does not affect any treatment other than that which would require intubation or CPR. Patients who are DNR can continue to get chemotherapy, antibiotics, dialysis, or any other appropriate treatments.
Death with Dignity [13]
[Palliative Medical Provisions, Article 7] In May 2000, the Taiwan legislature passed, and made public, this law, and has continued to make amendments up January 2013.
- Not performing cardiopulmonary resuscitation, or life sustaining medical treatment, shall meet the following requirements:
- Be certified by two physician as having a confirmed diagnosis of terminally ill
- Must have a living will signed by the patient himself. But when the patient signing the letter of intent is underage, it must be be also agreed to by his legal representative. When minors are unable to express their wishes, their legal representative must sign.
- The physicians mentioned in clause 1 of the preceding paragraph must have relevant specialist qualifications
- Cardiopulmonary Resuscitation (CPR)
- Refers to administering to patients who are end-of-life, dying or show no signs of life, any of endotracheal intubation, external cardiac compressions, emergency drug injection, extracorporeal membrane oxygenation (ECMO), cardiac shock, cardiac artificial pacemaker, artificial respiration or other standard resuscitation procedures other emergency treatment behavior.
- Vital Signs
- It means to maintain the terminally ill patient vital signs, but not to adminster any treatment that has no hope of healing, and would only prolong the dying process.
Do-not-resuscitate (DNR) orders have been in use in hospitals for over 20 years. Nonetheless, as currently implemented, they fail to adequately fulfill their two intended purposes:
- support patient autonomy
- prevent non-beneficial interventions
Problems with DNR orders in practice [2]
- DNR discussions occur too infrequently and patients' preferences regarding resuscitation are neglected.
- DNR discussions are delayed until it is too late for the patients to participate in decisions regarding resuscitation.
- Physicians do not provide adequate information to allow patients to make informed decisions.
- Physicians inappropriately extrapolate DNR orders to limit other treatments.
- Poor documentation of multiple DNR orders (rescinded and renewed by family)
Causes of poor implementation
- Medical culture values technology.
- Inadequate hospital policies on DNR discussion standards.
- Insufficient training of physicians in communication skills.
- Payment system that rewards volume and intensity of care (fee for service rather than fee for performance).
- Family and social pressure to perform CPR despite active DNR order
- RMO highest ranking medical officer dealing with family
Strategies for change
- Effective, comprehensive, hospital policy for DNR.
- Attending physician (not lower level RMO) to be responsible (conduct, sign) the discussion with patient and family/surrogate.
- Training of physicians in communication skills.
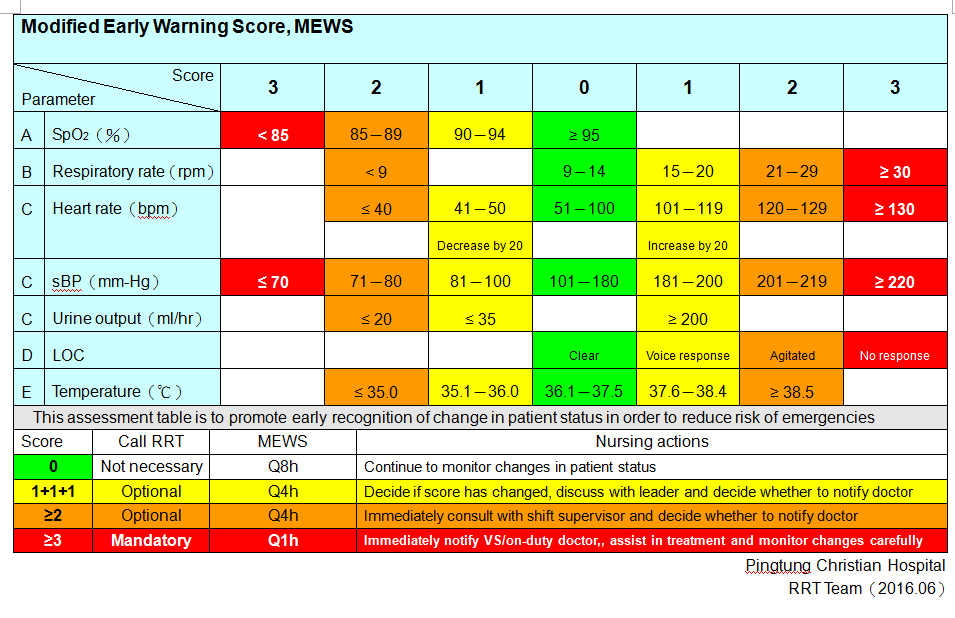
Modified Early Warning System (MEWS)
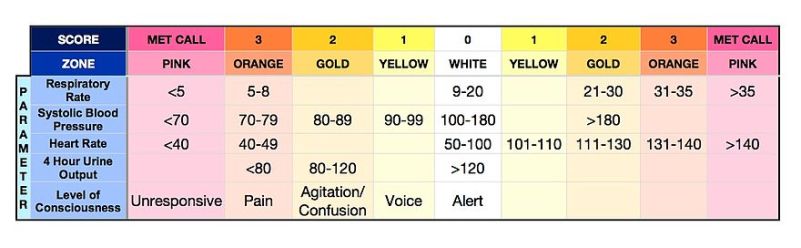
- A tool designed to identify patients with declining conditions
- Based on the priniciple that clinical deterioration can be seen through subtle changes in a number of parameters as well as large changes within a single variable.
- Scoring is based on: respiratory rate, heart rate, systolic blood pressure, temperature, SpO2, conscious level (AVPU response), hourly urine output. To accurately score blood pressure, the patient's usual or target blood pressure must be identified in order to calculate the BP score. The scale is calibrated to different populations and sometimes expanded to include additional parameters.
- A score is attributed to each observation based on the degree of physiological abnormality (see example above: figure 2). All of the observation scores are added together to provide a total MEWS.
- MEWS can be used on all hospitalized patients to allow for the early detection of clinical deterioration and potential need for higher level of care
- Patients with low MEWS can continue receiving their usual care and observation
- Patients with high MEWS can be watched more attentively and considered for transfer to a higher care unit such as an ICU
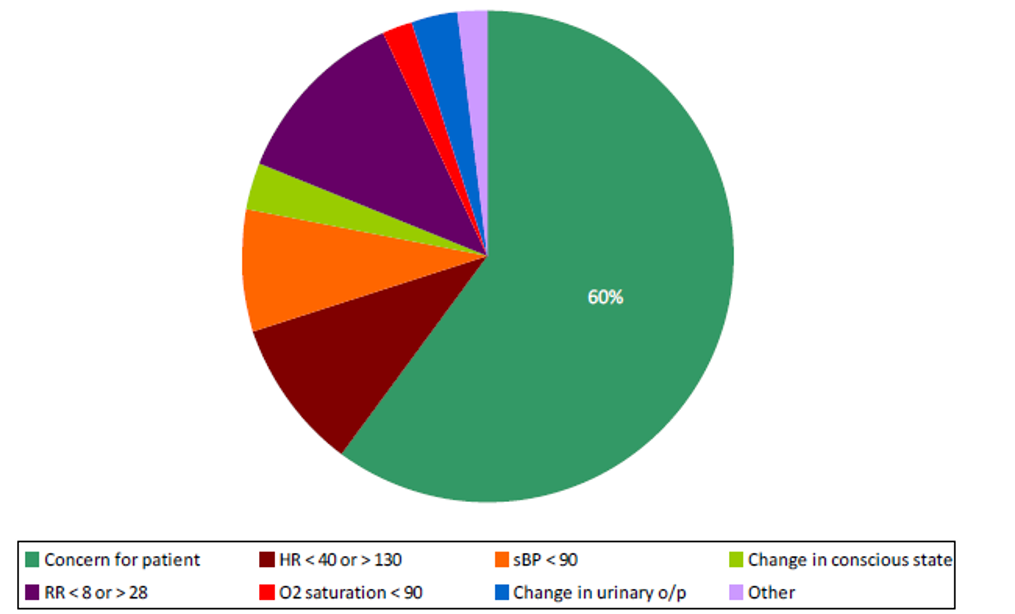
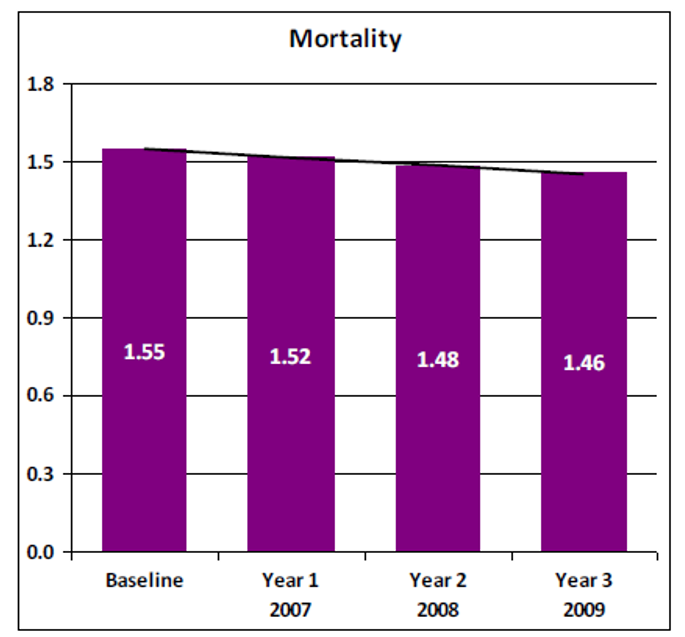
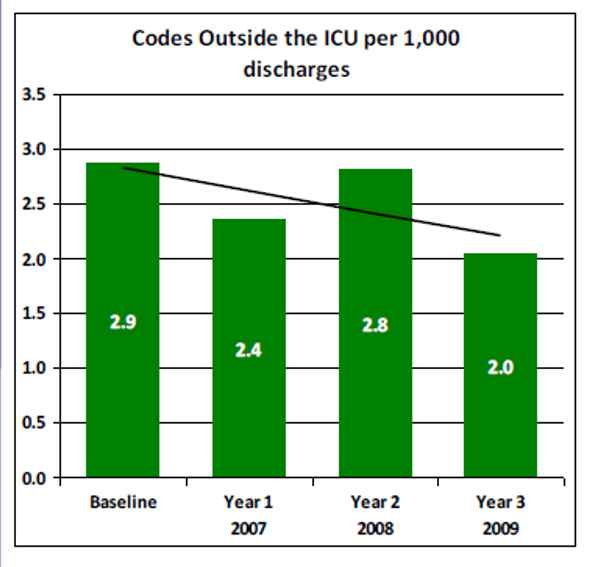
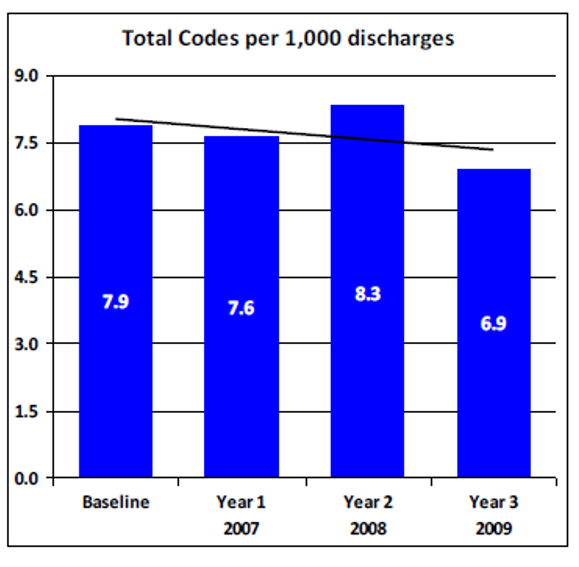
Example Results [16]
Mobile Nursing Station
A mobile nursing station is an innovative cart that integrates a wireless network, information technology devices, and online charts. In addition to improving clinical work and workflow efficiencies, data is integrated among different information systems and hardware devices to promote patient safety.

Examples of commercial products found online focus on information sharing (HIS/NIS) and look more like a laptop on a stand. In Asia, includes nursing functions (drugs, dressing changes etc) so drawers, waste bins, storage, lock, and bulkier. Problem: does it get between beds? Does it read data electronically/scanned?
Wifi blind spots. Electronically acquired: SpO2, BP, temperature, HR, respiratory rate, (urine output), patient bracelet for identification. HIPAA access to patient information; leaving station unattended but logged in... [15]
Charging (where, how often). Inoperative (power failure, screen burnout). Lapse in security when left unattended
Too sensitive MEWS: onduty doctor complains, nurse turns off or goes back to "old ways".

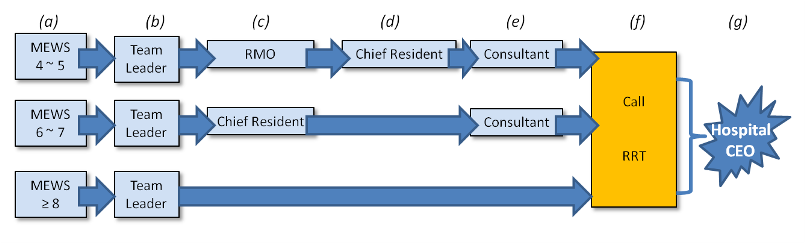
4. Activation/Escalation Protocol
The RRT may be called for physiologic changes in heart rate, systolic blood pressure, respiratory rate, pulse oximetry saturation, mental status or urinary output. Changes in laboratory values such as sodium, glucose and potassium could also indicate a patient’s condition is deteriorating.
The nurse may also call the RRT because of a gut feeling that all is not right.
Some hospitals have pioneered the use of Early Warning Scoring Systems to more reliably identify patients in trouble and trigger the appropriate, often lifesaving response. A standard communication system is set up to call the RRT so members can respond quickly — often within five minutes.
Any score greater than zero warrants increased surveillance of the patient. If the total MEWS reaches an initial trigger point (often set at four or five), the escalation protocol is initiated. It consists of two aspects:
Increasing frequency of observations
Half-hourly for the first hour (or more frequently if the patient's condition dictates)- If the MEWS falls to less than the preset trigger point (four or five), continue observations hourly for the next four hours, then every four hours for the next 24 hours.
- If there is no improvement in the MEWS or the patient continues to deteriorate: maintain on half-hourly observations or more frequently if clinically indicated.
Notify the relevant medical officer
To ensure that escalation is appropriate for the patient in the particular ward, the nurse notifies the team leader when a patient meets a trigger score according to the flowchart in figure 6. However:- If the patient meets the criteria for calling the RRT team, then this process should be activated.
- If the patient meets the criteria for calling the CPR team, then this process should be activated.
4a. Condition H
The University of Pittsburgh Medical Center (UPMC) Shadyside and Children’s Hospital appears to be the first facility in the U.S. to have invited patients and families to call for a RRT to address unresolved concerns about their safety and health. Upon admission, patients and family members are invited to pick up any phone in the hospital to report a Condition H (for "help") if they: [3][4][5]
- fear something is seriously wrong and have expressed their concerns without validating or recognizing its potential importance.
- experience a communication failure with the staff.
- become confused about the patient’s care.
- need to know where to voice concerns.
- feel something about the patient’s condition is "just not right"
Help is available around the clock. The phone call goes to the hospital operator, who pages the RRT. The team arrives at the patient’s bedside within minutes, listens to the patient’s or family member’s concerns, assesses the patient, and responds with medical care or further investigation, as needed.
Do families abuse the "call for help" system?
When the staff at Shadyside first introduced the idea of Condition H, many feared that too many calls would be made for non-urgent reasons, such as cold meals or uncomfortable pillows. The results of a pilot test, however, were positive, and the intervention was spread throughout the hospital.
Placing a picture of Josie King on the cover of the patient brochure that describes Condition H (also called the Josie King Call Line) and showing patients a video about this tragedy, when time permits, also acts as a deterrent to non-urgent calls. When patients see that the helpline is named after a child who lost her life because of medical errors, they are less likely to use the line to complain about food or other minor annoyances.
Between July 2005 and March 2006, Shadyside received 20 calls, mostly from patients. All calls were judged to have been appropriately initiated, and the hospital considers each call a learning experience. In fact, it is recognized that even though something interfered with communication between the patient, family, and staff, individuals should not be blamed. Condition H is considered an additional opportunity to step in before a tragedy occurs. However, Shadyside also believes that the program has caused staff members to ramp up their communication with patients. Patients say they feel much safer knowing they can get immediate attention if they feel they need it.
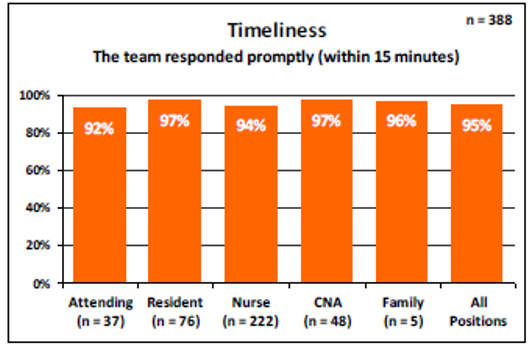
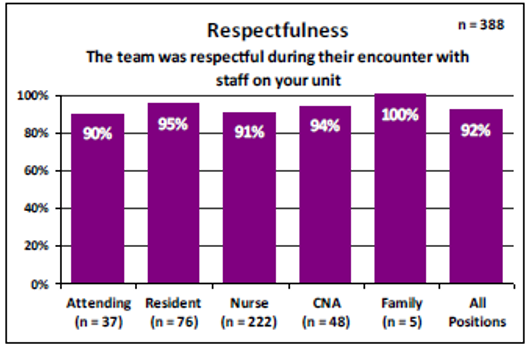
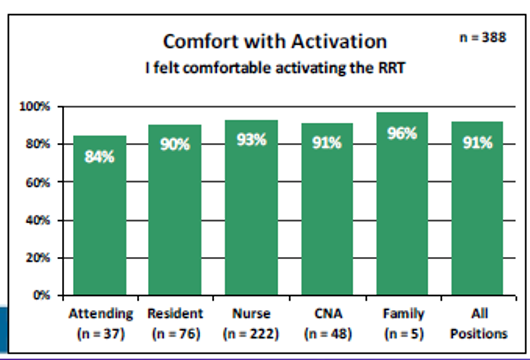
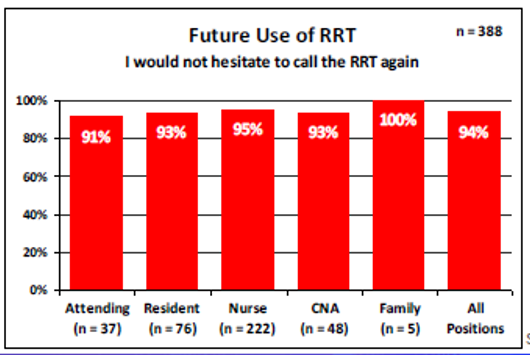
7. Staff Satisfaction
Example Rapid Response Team (RRT) staff satisfaction survey
Please answer the follow questions with respect to your encounter with the Rapid Response Team. {use 5-point Likert scale for each question}
Person completing the survey:
- The team responded promptly (within 15 minutes) Disagree ← → Agree
- The team was respectful during their encounter with staff on your unit Disagree ← → Agree
- The team provided help in clinical decision making while on the unit Disagree ← → Agree
- The patient's outcome was affected positively by the RRT being called Disagree ← → Agree
- I felt comfortable activating the RRT Disagree ← → Agree
- Overall the RRT was useful and beneficial Disagree ← → Agree
- I would not hesitate to call the RRT again Disagree ← → Agree
Any further comments or observations about the Rapid Response Team? {free text}
Example results of Survey [16]
8. CPR outside the ICU
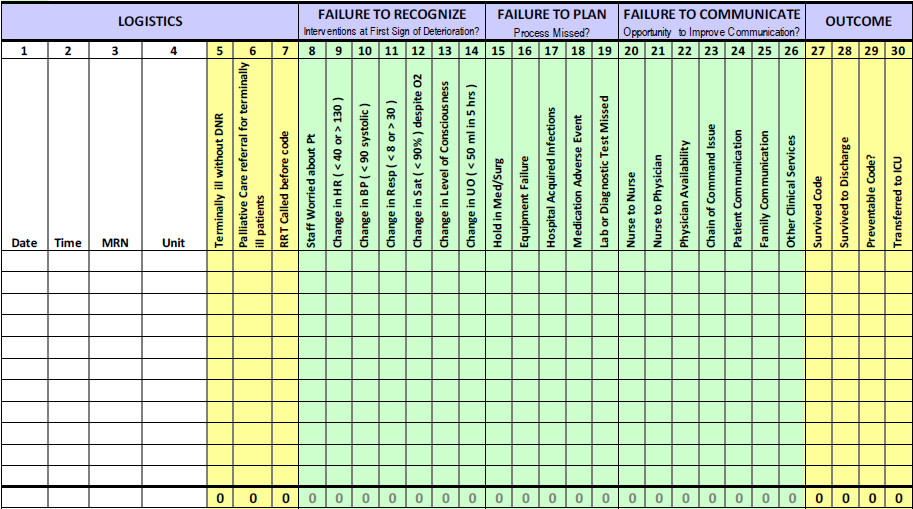
Scene investigation
RRT quality auditor completes chart revies on each code within 24 hours using this tool.
All codes outside the ICU must be reported using the table.
Date: _________ Time: __________ Unit: __________ Auditor: __________
|
FAILURE TO RECOGNIZE Interventions at first sign of deterioration? |
|
|---|---|
| 8. Staff worried about patient | ▢ |
| 9. Change in HR (<40 or >130) | ▢ |
| 10.Change in BP (<90 systolic) | ▢ |
| 11.Change in resp (<8 or >30) | ▢ |
| 12.Change in SpO2 (<90%) despite O2 | ▢ |
| 13.Change in level of consciousness | ▢ |
| 14.Change in UO (<50 mL in 5hr) | ▢ |
| FAILURE TO PLAN Process missed? |
|
| 15.Hold in Med/Surg | ▢ |
| 16.Equipment failure | ▢ |
| 17.Hospital acquired infections | ▢ |
| 18.Medication adverse event | ▢ |
| 19.Lab or diagnostic test missed | ▢ |
| FAILURE TO COMMUNICATE Opportunity to improve communication? |
|
| 20.Nurse to nurse | ▢ |
| 21.Nurse to Physician | ▢ |
| 22.Physician availability | ▢ |
| 23.Chain of command issue | ▢ |
| 24.Patient communication | ▢ |
| 25.Family communication | ▢ |
| 26.Other clinical service | ▢ |
| LOGISTICS | |
|---|---|
| 5.Terminally ill without DNR | Y◯ N◯ |
| 6.Palliative Care referral for terminally ill patients | Y◯ N◯ |
| 7.RRT called before CPR | Y◯ N◯ |
| OUTCOME | |
| 27.Survival code | Y◯ N◯ |
| 28.Survived to discharge | Y◯ N◯ |
| 29.Preventable code? | Y◯ N◯ |
| 30.Transferred to ICU | Y◯ N◯ |
RRT Performance Measures
Monthly Report on RRT Items
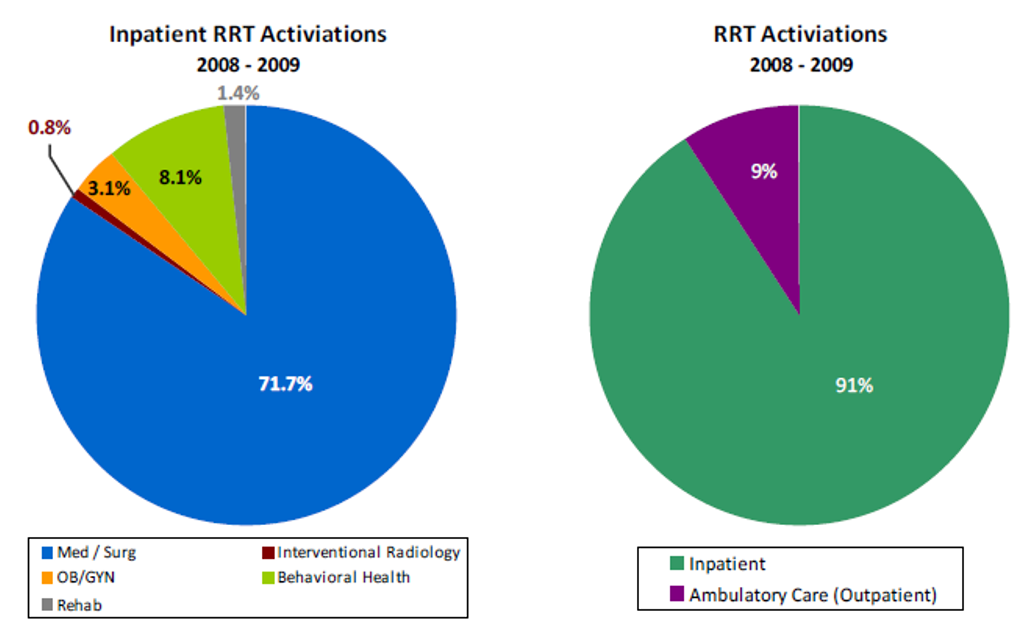
Although CPR occurs at outpatient and emergency departments, they do not have the opportunity of noticing patient changes during the preceding seven to eight hours, so are not part of this RRT design (they may be handled by existing CPR teams responding to code blue
calls, or some adaptation of the RRT concept which takes into account the environmental differences between inpatient wards and other areas of hospital care).

Data Dictionary
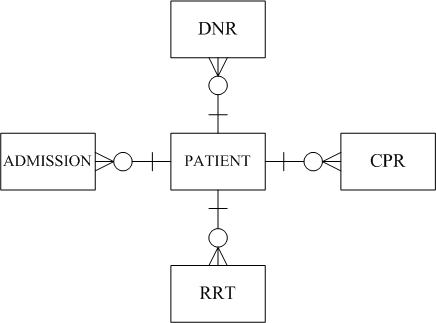
A person may have none, or one (thereby becoming a "patient"), or more than one, admission to hospital. During an admission, a patient may none, one, or more than one, of each of the following events: RRT, CPR, DNR.
| DNR | RRT | CPR | Audit |
|---|---|---|---|
| + | ? | — |
|
| + | ? | + |
|
| — | + | + |
|
| — | + | — |
|
| — | — | + |
|
| — | — | — |
|
Note that DNR orders can be cancelled and reinstated. Whether or not to effect CPR must take into account the patient's wishes as documented by the (currently active) DNR order.
Also, see the DNR section of this page to make sure that DNR does not mean "do not treat"!
Data Elements
Also, depending on your phase of implementation, stratify for each appropriate interval (indicator monitoring: monthly, quality improvement: daily)
| Code | Element |
|---|---|
| e-N | Number of inpatients discharged from hospital |
| e-WN | Number of inpatients discharged from hospital wards (outside ICU) |
| e-CPR-t | Number of times CPR was performed on {e-N} during inpatient stay |
| e-WCPR-t | Number of times CPR was performed on {e-WN} during inpatient stay |
| e-CPR-n | Number of patients in {e-N} who had CPR performed one or more times during inpatient stay |
| e-WCPR-n | Number of patients in {e-WN} who had CPR performed one or more times during inpatient stay |
| e-CPR-dnr | Number of times a DNR was in effect when each CPR in {e-CPR-t} was performed |
| e-RRT-t | Number of times RRT was activated for {e-WN} patients during the inpatient stay |
| e-RRT-n | Number of patients in {e-WN} who had RRT activated at least once during the inpatient stay |
| e-ICU-t | Number of times that patients in {e-WN} had an unplanned admission to ICU during the inpatient stay |
| e-?-d | Number of deaths at hospital discharge for: •all patients {e-N-d} •ward patients {e-WN-d} •all patients who underwent CPR {e-CPR-d} •ward patients who underwent CPR {e-WCPR-d} •ward patients who had RRT activated {e-RRT-d} |
| e-Team-t | Number of times the RRT members arrived "on-time" (within the designated interval) calculated from the time the RRT was activated in patients {e-RRT-t} until the documented arrival of the first team member at the patient bedside. |
Indicators
The MERIT study of RRT found no significant difference in cardiac arrests in patients without a do not resuscitate (DNR) order, unplanned ICU admissions and unexpected deaths taking place in general wards in those hospitals. However, American and Taiwan hospital accreditation encourage their use, as does the IHI "100 Lives" campaign. [f]
In the notes to the following indicators, I have quoted a few figures from the literature to give an idea of what indicator rates are seen in hospitals as they begin to implement an RRT program.
| Code | Name | Formula | Notes |
|---|---|---|---|
| RRT-1 | Total CPR events per 1,000 discharges {8a.QA} | 1,000 * ( e-CPR-t ÷ e-N ) | Total codes per 1,000 discharges: 7.9 {baseline} → 7.6 → 8.3 → 6.9 (17% reduction over 3 years) 17% decrease in the incidence of cardio pulmonary arrests (6.5 vs 5.4 per 1000 admissions) [DeVita et al [b] ] |
| RRT-1a | CPR events outside ICU per 1,000 discharges {8.QA} | 1,000 * ( e-WCPR-t ÷ e-WN ) ‰ | Codes outside the ICU per 1,000 discharges: 2.9 {baseline} → 2.4 → 2.8 → 2.0 (34% reduction over 3 years) 50% reduction in the occurrence of cardiac arrest outside the ICU [Buist et al [c] ] |
| RRT-2 | Hospital mortality {10.QA} | ( e-N-d ÷ e-N ) % | Hospital mortality: 1.55% {baseline} → 1.52% → 1.48% → 1.46% [Lives saved: 659] [Gadkar et al [16] ] |
| RRT-2a | Mortality rate at discharge for CPR patients {8a.QA} | ( e-CPR-d ÷ e-CPR-n ) % | ?? |
| RRT-2b | Mortality rate for ward CPR patients {8.QA} | ( e-WCPR-d ÷ e-WCPR-n ) % | ?? |
| RRT-3 | Number of unplanned ICU admissions {9.QA} | ( e-ICU-t ÷ e-WN ) % | Decrease in the number of unnecessary transfers to a higher level of care by a mean of 30% [Goodhill et al [d] ] Severe postoperative adverse events (i.e., respiratory failure, stroke, severe sepsis, acute renal failure) were reduced by 58%, emergency ICU admissions were reduced by 44%, postoperative deaths were reduced by 37%, and mean duration of hospital stay decreased from 23.8 to 19.8 days in surgical patients [Bellomo et al [e] ] |
| RRT-4 | Staff satisfaction {7.QA} | % | Staff satisfaction with the benefits of RRT service high (90%~100%) for all 6 job categories |
| RRT-5 | CPR on DNR patients per 1,000 discharges {3a.QA} | ( e-CPR-dnr ÷ e-N ) ‰ | ?? |
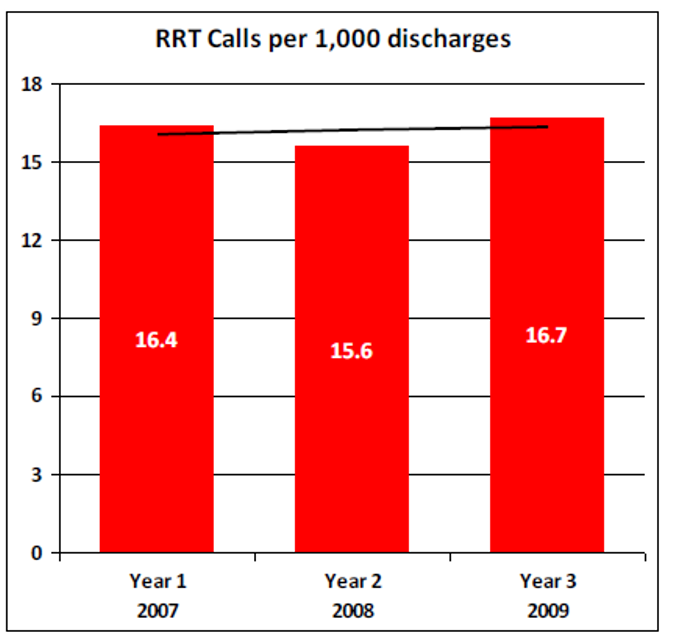
| RRT-6 | RRT activations per 1,000 discharges {4.QA} | ( e-RRT-t ÷ e-N ) ‰ | RRT calls per 1,000 discharges: 16.4 → 15.6 → 16.7 [Gadkar et al [16] ] |
| RRT-7 | Express handover (SBAR) compliance {6.QA} | ( e-RRT-t ÷ e-WN ) % | ?? |
| RRT-8 | Response time compliance {5.QA} | ( e-Team-t ÷ e-RRT-t ) % | ?? |
Related References
-
MERIT study investigators.
Introduction of the medical emergency team (MERIT) system: a cluster-randomised controlled trial.
Lancet 2005; 365(9477): 2091-2097 -
DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL.
Use of medical emergency team responses to reduce hospital cardiopulmonary arrests.
Quality and Safety in Health Care 2004; 13(4): 251-254 -
Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV.
Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study.
BMJ 2002; 324: 387 -
Goodhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A.
The patient-at-risk team: identifying and managing seriously ill ward patients.
Anaesthesia 1999; 54(9): 853-860 -
Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, Silvester W, Doolan L, Gutteridge G.
Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates.
Critical Care Medicine 2004; 32(4): 916-921 -
Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD.
The 100,000 Lives Campaign: Setting a goal and a deadline for improving health care quality.
[ Journal of the American Medical Association] 2006;295(3):324-327.
References:
- Prince Charles Hospital, Queensland Health. Modified Early Warning Score (MEWS), Escalation and ISBAR www.safetyandquality.gov.au (pdf:5pp)
- Yuen JK, Reid MC, Fetters MD. Hospital Do-Not-Resuscitate Orders: Why They Have Failed and How to Fix Them www.ncbi.nlm.nih.gov J Gen Intern Med. 2011; 26(7): 791–797.
- Grissinger M. Rapid Response Teams in Hospitals Increase Patient Safety www.ncbi.nlm.nih.gov P T. 2010; 35(4): 191, 207.
- Institute for Healthcare Improvement: Open School The Josie King story www.ihi.org
- Louis Blackman story www.youtube.com
- MERIT study investigators. Introduction of the medical emergency team (MERIT) system: a cluster-randomised controlled trial. www.thelancet.com Lancet 2005; 365(9477): 2091-2097
- DeVita MA, Braithwaite RS, Mahidhara R, Stuart S, Foraida M, Simmons RL. Use of medical emergency team responses to reduce hospital cardiopulmonary arrests. pubmed.ncbi.nlm.nih.gov Qual Saf Health Care 2004; 13(4): 251-254
- Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. www.bmj.com BMJ 2002; 324: 387
- Goodhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at-risk team: identifying and managing seriously ill ward patients. pubmed.ncbi.nlm.nih.gov Anaesthesia 1999; 54(9): 853-860
- Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, Silvester W, Doolan L, Gutteridge G. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. pubmed.ncbi.nlm.nih.gov Crit Care Med 2004; 32(4): 916-921
- Berwick DM. Overview of the 100,000 Lives Campaign www.ihi.com 2pp
- Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100,000 Lives Campaign: Setting a goal and a deadline for improving health care quality. www.ihi.org Journal of the American Medical Association. 2006;295(3):324-327.
- Cook D, Rocker G. Dying with Dignity in the Intensive Care Unit www.nejm.org N Engl J Med 2014; 370:2506-2514
- Wikiwand. Early warning score www.wikiwand.com
- U.S. Department of Health & Human Services Summary of the HIPAA Privacy Rule www.wikiwand.com
- Gadkar N, Williams R, Russon M. Rapid Response Teams: Do We Need Them? New York City Health & Hospitals Corporation www.nychhc.org April 2016 (presented at conference).


