Rationale
The definition of an adverse event can vary widely, for example a patient safety incident as used by the NHS in the UK, includes incidents that result in no harm and incidents that are caught before they reach the patient. In comparison, the Harvard Medical Practice Study's methodology used in retrospective chart review studies in several countries considers adverse events to be injuries resulting in prolonged hospitalization, disability or death, which are caused by healthcare management; thereby filtering out the minor and minimum levels of harm events.
The root causes of all adverse events, including near misses, show the same underlying patterns of failure. High reliability industries such as the aviation industry treat near misses and minor adverse events as rigorously as those that result in death or permanent disability. By addressing near misses and minor advers events, the underlying causes can be corrected before they lead to a disastrous incident.
- Adverse Event
- An undesirable clinical outcome that has resulted from some aspect of diagnosis or therapy, not an underlying disease process. Preventable adverse events are the subset that are caused by error. [14]
- Error
- An act of commission (doing something wrong) or omission (failing to do the right thing) that leads to an undesirable outcome or significant potential for such an outcome. [14]
- Near Miss
- an error of commission or omission that could have harmed the patient, but serious harm did not occur as a result of [8]
• chance (e.g. the patient received a contraindicated drug but did not experience an adverse drug reaction)
• prevention (e.g. a potentially lethal overdose was prescribed, but a nurse identified the error before administering the medication)
• mitigation (e.g. a lethal drug overdose was administered bu discovered early and countered with an antidote)
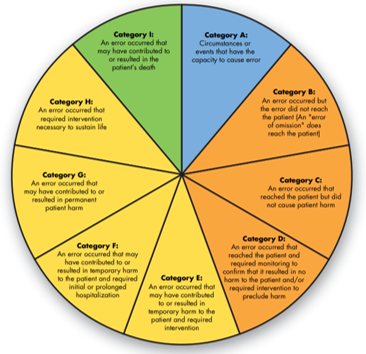
NCC MERP INDEX
Near Miss (lack of consensus)
-
the WHO definition includes events that REACH the patient (provided no harm was experienced)
→ B~D in Figure 2 above -
the CMIRPS definition includes only occurrences that DO NOT REACH the patient
→ B in Figure 2 above
-
A: Blue: no error.
- Category A: Circumstances or events that have the capacity to cause error.
-
B~D: Orange: Error, no harm.
- Category B: An error occurred but the error did not reach the patient (an 'error of omission' does reach the patient.
- Category C: An error occurred that reached the patient but did not cause patient harm.
- Category D: An error occurred that reached the patient and required monitoring to confirm that it resulted in no harm to the patient and/or required intervention to preclude harm.
-
E~H: Yellow: Error, Harm
- Category E: An error occurrred that may have contributed to or resulted in temporary harm to the patient and required intervention.
- Category F: An error occurred that may have contributed to or resulted in temporary harm to the patient and required initial or prolonged hospitalization.
- Category G: An error occurred that may have contributed to or resulted in permanent patient harm.
- Category H: An error occurred that required intervention necessary to sustain life.
-
I: Green: Error, Death.
- Category I: An error occurred that may have contributed to or resulted in the patient's death.
Severity Assessment Code (SAC) Matrix
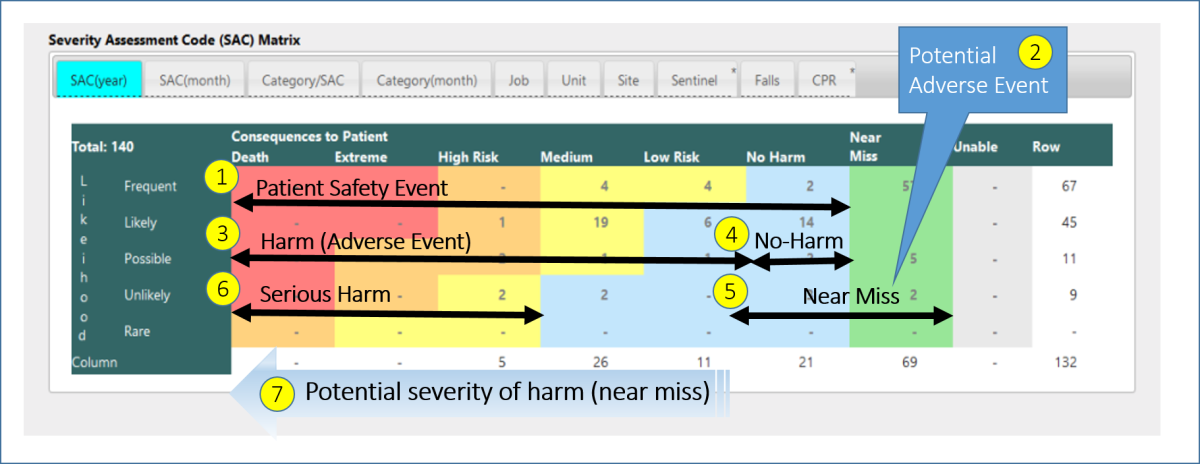
Legend to Figure 2 SAC Matrix
| SAC-1 | Extreme Risk | (immediate action) | resulted in death or permanent disability of the patient |
| SAC-2 | High Risk | (senior management attention needed) | As well as needing additional medical resources, requires hospital admission or extension of stay in hospital for special treatment |
| SAC-3 | Medium Risk | (management responsibility must be specified) | Requires additional medical resources, assessment, or observation, but only needs simple treatment such as blood transfusion, urine examination, ligation, or stopping hemorrhage. |
| SAC-4 | Low Risk | (manage by routine procedures) | aggregate data then undertake a practice improvement project: the incident caused harm but did not require additional medical resources |
| SAC-5 | No Harm To Patient | The adverse event reached the patient but did not cause any harm | |
| SAC-6 | Not To Patient | because of inattention or immediate action, a possible adverse event was prevented from reaching the patient |
| 1 | Patient Safety Event | a safety event that reached the patient. |
| 2 | Potential Patient Safety Event | a safety event that did not reach the patient. |
| 3 | Harm | Harm caused by the patient safety event; further classified by severity using either the SAC matrix here, or the Merp index (E~I). An impairment of structure or function of the body and/or any deleterious effect arising therefrom, including disease, injury, suffering, disability, and death. Harm may be physical, social, or psychological, and either temporary or permanent. |
| 4 | Near Miss | The total absence of physical and psychological injury to patients and the workforce. [ACHE] |
| 5 | No Harm | a potential patient safety event (same as #2) |
| 6 | Serious Harm | documented harm resulting in death, permanent injury, increased hospital expenses, as in the Harvard and Australian studies. |
| 7 | Potential harm severity (near miss) | as in RCA^2 to decide if catastrophic results might have occurred, the indication for a Root Cause Analysis. |
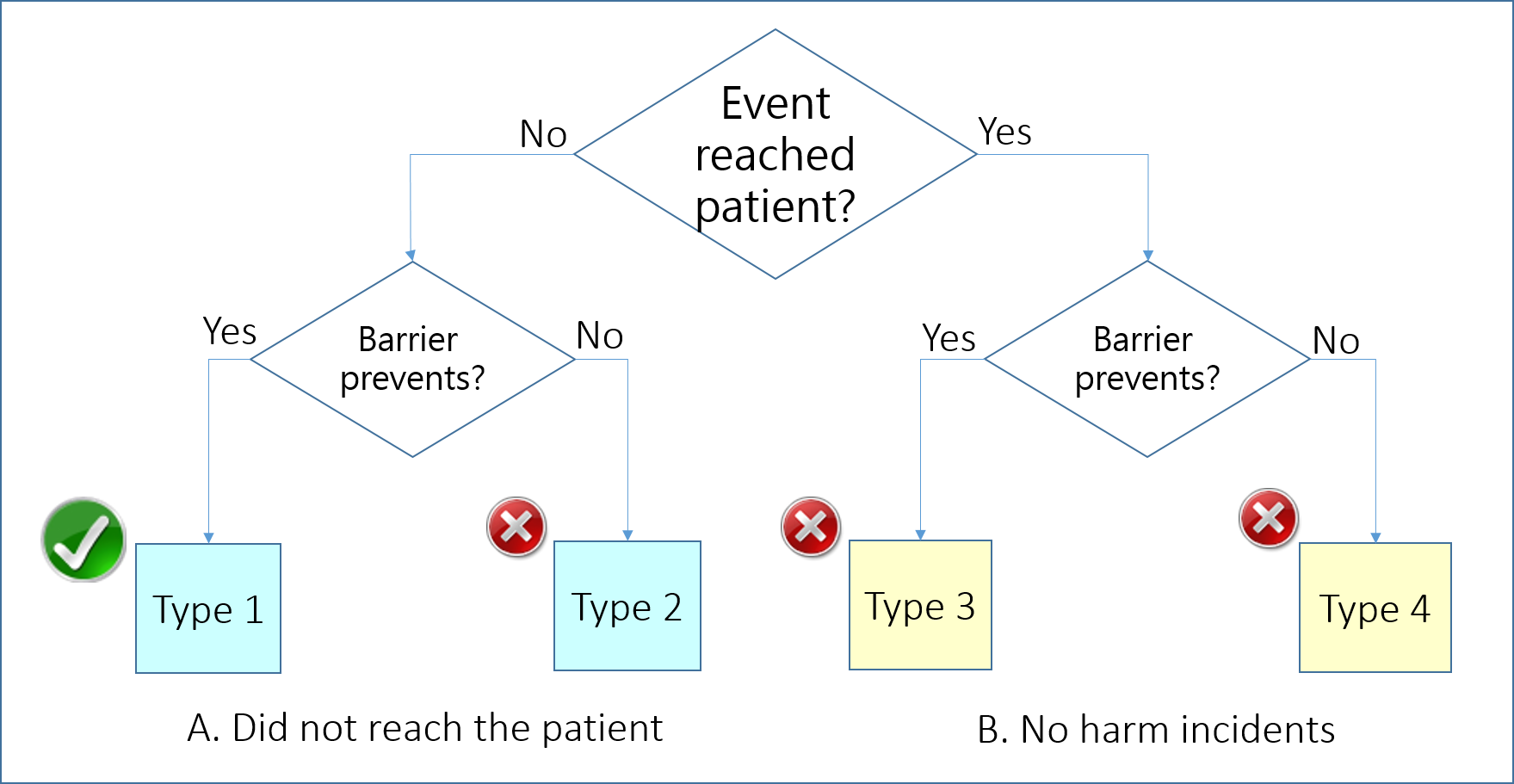
Near Miss
- an error that has the potential to cause an adverse event (patient harm) but fails to do so because of chance or because it is intercepted [4]
- an act of commission or omission that could have harmed the patient but did not cause harm as a result of chance, prevention, or mitigation [3]
- an error caught before reaching the patient [5]
Some definitions emphasize that a near miss is an incident that did not reach the patient at all because it was intercepted before reaching the patient; however, others emphasize that a near miss may reach the patient but does not cause harm [7] or does not cause serious harm [8] .
-
Type 1: not indicative of organizational weakness.
They indicate that the predetermined plans and actions are correct. Therefore, collect information to evaluate the effectiveness of such plans. -
Type 2~4: indicate a weakness of the healthcare system (organization) for designing appropriate formal measures to prevent the continuation of the events.
- Type 2 near misses help healthcare organizations to identify effective unplanned and accidental actions and make decisions to formalize them.
- Type 3 help to evaluate detection and intervention procedures and increased use of resources for detecting and mitigating the events.
- Type 4 show the weakness of the organization in early detection of events after reaching to the patient.
Both subgroups should be assessed for severity. For the first subgroup (reached patient), assign severity based on the patient's actual condition. For the second group (did not reach patient), assign severity based on a reasonable worst case
systems level scenario.
Each of these four types of incidents provide different information and viewpoints about healthcare errors, and error management practices. Near misses and no harm incidents can provide valuable information much of which cannot be captured by adverse event reporting systems, therefore, reporting such incidents should be encouraged; however, necessity of developing a large database and employing more staff for data management should also be considered.
Medication Error
psnet.ahrq.gov
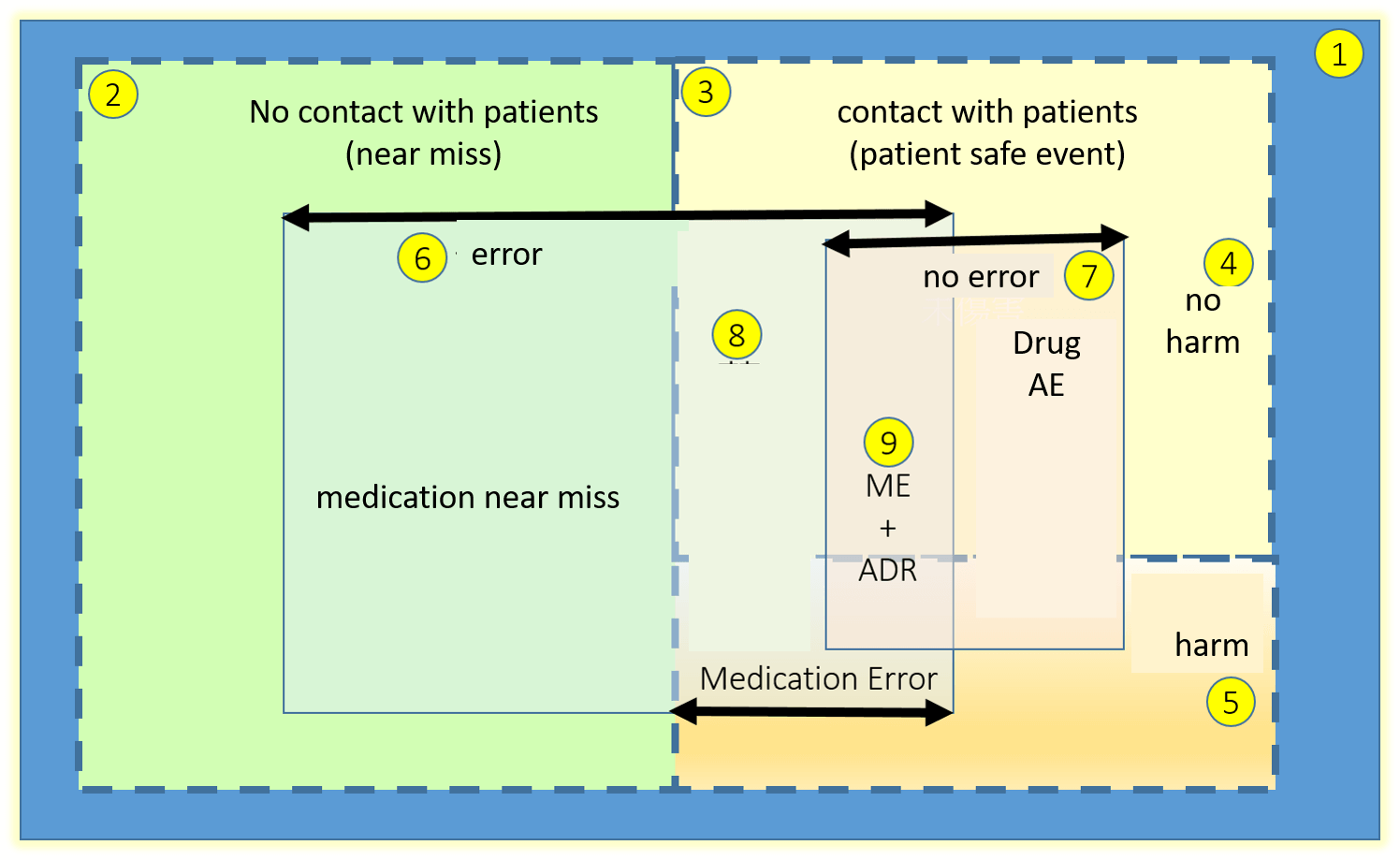
- World (blue background)
- Did not reach the patient (green background)
- Reached the patient: (pale yellow background {3} and orange gradient background {4})
- No harm: (pale yellow background)
- Harm (orange gradient background {4)}
- Error (pale blue bacground, crossing {2} and {3}
- No error: adverse drug reaction (ADR) (pale pink background, crossing {4} and {5})
- Medication "error" (the part of {6} in {4} and {5})
- ME+ADR: common area to {7} and {8}
- Adverse drug event (ADE)
-
harm experienced by a patient as a result of exposure to a medication. As with the more general term 'adverse event', the occurrence of an ADE does not necessarily indicate an error or poor quality care.
A certain percentage of patients will experience ADEs even when medications are prescribed and administered appropriately; these are considered adverse drug reactions (ADR) or nonpreventable ADEs. - Medication error (ME)
- an error (of commission or omission) at any step along the pathway that begins when a clinical prescribes a medication and ends when the patient actually receives the medication. These are all considered preventable.
International Trends
International retrospective reviews of patient charts estimated that between 4% and 17% of hospital admissions were associated with an serious adverse event (subgroup 1 above) and a significant proportion of these (one- to two-thirds) were preventable. London and Scotland hospitals found a rate of about 10%; other countries (USA, Australia, UK, New Zealand, Canada) found a median overall incidence of adverse events of 9.2% (of which approximately 43% were preventable), with over half being surgical (40%) or drug (15%) related. Older patients and those with multiple co-morbidities are at higher risk of suffering an adverse event. Although most adverse events resulted in little or no disability, a significant minority (median 14%) caused permanent disability (7%) or death (7%).
Incident reporting systems (IRS) collect only a small proportion of adverse events (around 1-10%), which are not representative of all adverse events (70% of IRS reports are falls, pressure ulcers and drug related events whereas these constitute only 26% of adverse events detected by retrospective review of medical charts).
- Incident
- An incident can refer to any event that happens; it could be positive or negative. If the event is negative (an unplanned, undesired event that hinders completion of a task and may cause injury, illness, or property damage or some combination of all three in varying degrees from minor to catastrophic), it is called an 'adverse event'.
- Unplanned and undesired do not mean unable to prevent.
- Unplanned and undesired also do not mean unable to prepare for.
- Crisis planning is how we prepare for serious incidents that occur that require response for mitigation.
- Accident
- The definition is often similar to incident, but supports the mindset that it could not have been prevented. An accident is the opposite of the fundamental intentions of a safety program, which is to find hazards, fix hazard, and prevent incidents. When we accept that accidents have no cause, we assume that they will happen again.
References
- IHI & NPSF. Patient Safety Dictionary A~E www.npsf.org
- IHI & NPSF. Patient Safety Dictionary F~M www.npsf.org
- IHI & NPSF. Patient Safety Dictionary N~Z www.npsf.org
- IHI & NPSF. Patient Safety Definitions Source List www.npsf.org
- Sheikhtaheri A. Near Misses and their importance for improving patient safety. www.ncbi.nlm.nih.gov Iran J Public Health. 2014; 43(6): 853-854.
- National Patient Safety Foundation. RCA2: Improving Root Cause Analyses and Actions to Prevent Harm. www.npsf.org .2015
- Aspden P. Patient safety: achieving a new standard for care. Institute of Medicine; USA. 2004.
- World Alliance for patient Safety. WHO draft guidelines for adverse event reporting and learning systems: from information to action. psnet.ahrq.gov World Health Organization, Geneva. 2005.
- Aston E, Young T. Enhancing the reporting of "near miss" events in a children's emergency department. ac.els-cdn.com J Emerg Nurs, 2009; 35(5): 451–452.
- Kessels-Habraken M, Van der Schaaf T, De Jonge J, Rutte C. Defining near misses: Towards a sharpened definition based on empirical data about error handling processes. www.ncbi.nlm.nih.gov/pubmed/ Soc Sci Med, 2010; 70(9): 1301–1308.
- Lamb BW, Nagpal K. Importance of near misses doi.org/10.1136/bmj.b3032 BMJ, 2009; 339(3):b3032.
- Wu A, Morlock L. Adverse events and safety in hatleh care: concepts and definitions ocw.jhsph.edu/courses/PatientSafety/ Johns Hopkins University, 2008.
- 13. ISMP Canada Safety Bulletin. Near Miss Identification and Reporting www.ismp-canada.org ISMP Canada, 2007.
- [ACHE] reference