For information collected to be used effectively, the investigation team will need to ensure that their information is complete and validated.
The key first step is to determine the chronology of the incident.
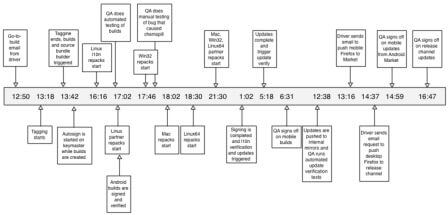
What is a Timeline?
A timeline is a method for mapping and tracking the chronological chain of events involved in the incident. It allows the investigator(s) to identify information gaps and also to identify critical problems that arose during the process of care delivery. The usual presentation of the timeline is via the diagrammatic formats detailed below. The data confines itself to the critical path, and does not detail any of the other salient points that might give an indication of the prevailing circumstances at the time. This supplementary information can be added once the critical path has been mapped.
When to use a Timeline
- when undertaking any incident investigation, either as an individual or a team, where it is anticipated that the incident contains more than one isolated episode of procedural failure
- when the timeline (chronology) needs to be mapped prior to a RCA (Root Cause Analysis) meeting with those involved in the incident, so that the way that the incident unfolded can be shown in an easily accessible format
- useful to map an incident when you have multiple specialities or agency involvement (e.g. homicide, community care suicide, Part 8 reviews), as it allows the systematic mapping of a variety of narrative chronological reports as well as mapping the interface between the various agencies involved in the care or case management. However in such cases modifications to the timeline will be required. (See Tabular Timeline).
How to complete a Timeline
A timeline should either begin at the point at which the chain of events leading to the incident started, or at the point of incident occurrence and work backwards to the agreed start point. Whichever method is used, it is easier for potential readers of the timeline to have it presented in chronological order leading up to the incident. For most acute secondary care cases the time frame will span at least the period of admission to incident occurrence, though there will be occasions where the pre-treatment period needs to be included. However for community based incidents, or where multiple agencies are involved, or if there is any uncertainty at all about where the ‘ball started to roll’, it is best to start with the incident and map the chain of events backwards, until you, and your team, are satisfied that you have either identified the initiating event(s), or have encompassed enough ‘history’ to enable a credible review to be undertaken. It is important to be realistic when deciding how far back to go and, you will need to apply the principle of what is reasonable and what may be helpful in terms of the investigation.
Owing to the nature of data collection you do not have to wait until you have complete information before starting to map your timeline, as information can be added to the timeline as and when it becomes available. Each event identified, including the date or time of its occurrence should be placed in a box in chronological order. Arrows indicating the direction of time should link the boxes. Any supplementary information can be linked to the primary time-stamped event box.
Positive attributes of the Timeline
- gives you greater clarity about the key components of the incident chain, along with the supporting contextual information (compared to some other techniques)
- allows you to view the whole incident in one diagram
- helps identify information gaps and questions needed for interviews
- experience suggests that investigators and staff using timelines are better able to identify the CDPs/SDPs (Care Delivery Problems/ Service Delivery Problems) that may require further causal analysis
- enables you to make sense of complex and convoluted data.
Negative attributes of the Timeline
- for some cases, which span a long period of time e.g. mental health cases, timelines can become very long and unwieldy
- depending on your level of computer literacy, it can be difficult to integrate timelines into final reports easily.
Mapping
Gather information and establish a chronology of the events. Considerable information needs collating to support the investigation. In order to make sense of the evidence obtained, information mapping is undertaken. Information mapping is a simple method of organising evidence submitted; examples of informations methods are:
- Narrative Chronology: An account of what happened in date, time order. It is constructed using information that has been collected from a number of difference sources into one account of the incident being investigated.
- Time Person Grid: Enables a close analysis of concentrated time periods when the investigating team need to understand precisely who was doing what and where. Each column of a table represents a defined period of time (five minute intervals, ten minute intervals). This makes it easier to check one person's actions throughout an incident, or to see what each individual was doing at one specific point in time.
- Tabular Timeline: Is mapped in a table format and provides an opportunity to record for each event the nature of the event; the date; the time; supplementary information (if available); good practice (where identified) and care or service delivery problems. The table allows more detail to be recorded, as well as some early analysis but retains the discipline of the chronology.
Examples of a Narrative Chronology
25 August 2003
10:30 Domiciliary visit undertaken by Dr Taylor
15:30 Mr Klein admitted on an informal basis to ward 7
16:45 Mental health assessment undertaken by Staff Nurse Woods, who found him depressed in mood
17:40 Mr Klein was sitting in lounge
17:55 Mr Klein threw a cup of coffee over Healthcare support worker Bull
26 August 2003
09:30 Mr Klein assessed by multidisciplinary team
Example of a Time-Person Grid
What is a Time-Person Grid?
A time person grid is a tabular mapping tool that enables you to track the movements of people (staff, patients, visitors, contractors) before, during and after an incident, therefore enabling the investigator to clarify where all persons were at key points in the incident.
When to use a Time-Person Grid
- when you have a number of personnel involved in an incident and you need to ascertain where they were as the incident was occurring. (e.g. child abduction case, absconsion case, unexpected clinical emergency, violence and aggression)
- it is particularly useful for short time frames when a lot seems to be going on and many people are involved in the delivery of care. This tool enables you to clarify timings and placement of people and identify areas requiring clarification
- a time person grid can be mapped onto a timeline to examine a specific time frame in more detail. It is unlikely that you would use a time person grid for the whole of an incident, unless it is very short e.g. less than 30 minutes.
Positive attributes of the Time-Person Grid
- it is a quick and efficient tool to identify where all staff were when events within an incident were happening
- a useful mechanism for identifying where you have data or information gaps
- it maps onto a timeline effectively.
Negative attributes of the Time-Person Grid
- it can only be used for short timeframes
- people cannot always remember where they were at specific times, especially if the case did not seem particularly significant to them at the time
- focuses on individuals.
How to complete a Time-Person Grid
- Create a table composed of a number of rows and columns, see Figure below.
- In the furthest column on the left list all the staff involved in the incident. Title this column [staff involved] or something similar.
- The following column headings should be time stamped e.g. 9.00, 9.05. 9.10, etc. These must run for the duration of your incident, or for the period you have decided to analyse using this technique.
- At each point in time, ascertain where each member of staff was e.g. at 9.10, anaesthetist was in the anaesthetic room.
| Staff | 12:05 | 12:15 | 12:25 |
|---|---|---|---|
| Senior Nurse A | With patient 1 | With patient 3 | At Nurse Station |
| Receptionist | With patient 2 | ? | At Nurse Station |
| Health Visitor | With patient 1 | With patient 1 | At Nurse Station |
| Doctor 1 | ? | ? | With patient 2 |
Example of a Tabular Timeline
What is a Tabular Timeline?
This is a development of the simple Timeline, which includes more than just the basic facts. For each event, as well as its nature, date and time, there are three other fields that can be completed if the team has this information. These are Supplementary Information; Good Practice; and Care Delivery Problem/Service Delivery Problem. The table allows more detail to be recorded, but retains the discipline of the timeline type chronology.
When to use a Tabular Timeline?
A tabular timeline can be used for any type of incident. However, experience has shown that it is particularly useful for incidents that involve a long time scale and those in primary care and mental health. This approach is also useful when multiple agencies are involved in an incident, for example a review of a child abuse case, where there is a lot of information to cross-reference.
Positive attributes of the Tabular Timeline?
- allows the investigation team to map the chronology in a diagrammatic format, but allows additional information (e.g. CDP/SDP, supplementary information and good practice) to be mapped at the appropriate point on the chronology. This makes the technique easy to read and resource efficient
- technique allows identification of data gaps quickly
- additional information can be added where needed, without the need of reformatting.
Negative attributes of the Tabular Timeline?
- some people prefer to map a case in a more fluid and dynamic way than this format allows.
How to complete a Tabular Timeline?
A tabular timeline will initially be completed in exactly the same way as a diagrammatic timeline, where the event date and time are completed in the first two boxes of the table. Please note that date and time can be supplemented with a generic term like day or month if it is considered more appropriate (this may often be appropriate for cases that have a long tail e.g. learning disabilities, primary care). When reviewing events over long periods of time, detailing exact dates and timings may not be necessary. Month of occurrence can be used instead.
Once the core information has been plotted, any other supplementary information, good practice or Care Delivery / Service Delivery Problems can be recorded in the dedicated rows assigned to them.
- Event date and time
- Event
- Care Delivery Problem (CDP) / Service Delivery Problem (SDP)
- Supplementary information
- Good Practice
| DateTime | 18 May 2009 09:25 | 18 May 2009 10:15 | 18 May 2009 11:05 |
| Event | Patient admitted to the ward by Duty Doctor | Patient admitted by Primary Nurse | Patient reviewed in clinical team meeting |
| Problem | Nursing admission not completed | ||
| Contributory Factor | Patient abusive during physical examination | ||
| Good Practice | Medical Notes fully completed | Patient observed as requested |