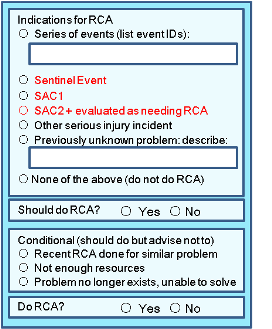
The decision to carry out a root-cause analysis will normally be because of one of the following:
Sentinel Events (single event): require RCA by definition.
-
Unanticipated death, including, but not limited to
- death that is unrelated to the natural course of the patient's illness or underlying condition (for example, death from a postoperative infection, a hospital-acquired pulmonary embolism, a mediction error leading to death
- death of a full-term infant
- maternal death associated with labor or delivery
- suicide
- Major permanent loss of function unrelated to the patient's natural course of illness or underlying condition
- Specific events designated as sentinel events
- Surgery events:
- Procedures involving the wrong patient, wrong site, or wrong procedure
- Retained instruments
- Unintended material requiring surgical removal
- Transmission of a chronic or fatal illness as a result of infusing blood or blood products or transplanting contaminated organs or tissues
- Hemolytic blood transfusion
- Infant abduction or discharge to wrong family
- serious maternal morbidity associated with labor or delivery
- {JCI:2014} rape, workplace violence such as assault (leading to death or permanent loss of function); or homicide (willful killing) of a patient, staff member, practitioner, medical student, trainee, visitor, or vendor while on hospital property.
- Risk (near miss) of any of the above
- Surgery events:
Non-Sentinel Events:
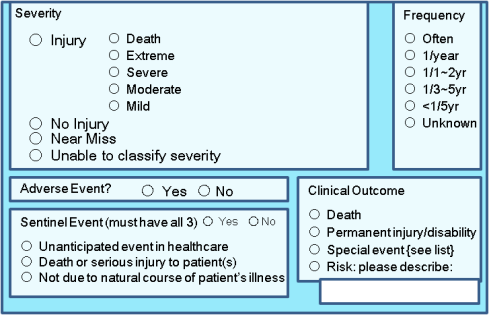
- The severity of the adverse event — can be assessed by direct observation. (A number of risk assessment indices have been developed to help in making the decision e.g. Severity Assessment Code 1 or 2 is an indication for RCA, even if not the event was not one of the sentinel events listed above).
- Series (multiple occurrences of the same event): The likelihood of recurrence of similar adverse events — series of recurrences for which more detailed analyses were not carried out on individual incidents may lead to improvements in the delivery of care from aggregate analysis of the series as a whole, rather than one by one. This assessment is facilitated by access to a database of incident reports.
Constraints (meets criteria for RCA but RCA not performed)
- Whether a similar case has been investigated recently — full root-cause analysis will have only marginal usefulness.
- The resources available to carry out such analyses — a judgment call for the patient safety team.
- The potential for correction — depends on the expertise of the patient safety team.
Incident Reporting System: partially-automated decision/documentation process for RCA (intranet)
Should we do an RCA for ALL adverse events?
It is not feasible to do an RCA for all individual adverse events and near misses, only a subset. Otherwise:
- useless analyses will be carried out because there is no time to do them properly
- effort will be devoted to performing analyses at the expense of testing and implementing real system changes that can reduce injury rates
Questions to Ponder
- Where to draw the line when assessing the "risk" of an adverse event? If not careful, the entire database of incident reports could become inappropriately overweighted in incidents subjectively assessed as "severe" by managers with unequal training.
- If a near miss is rated as having the "risk of death", is it still a near miss, or should it be reclassified as SAC=type 1 because of its potential severity?
- Some expert panels consider endotracheal dislodgement as a "moderate risk" in all cases. Is there no difference in risk for patients who need to be reintubated (clinical condition presumably poor if undergoing appropriate clinical care) and those who do not need to be reintubated (presumably because intubated for longer than necessary). Moreover, if those who are reintubated are at poor risk (many die), why does is the recommended grade only as "moderate risk"?