- What are we trying to accomplish? (Aim statement)
- How will we know that a change is an improvement? (Measures)
- What changes can we make that will result in improvement? (Changes)
The Model for Improvement
[1] is a simple framework for accelerating improvement.
It consists of two parts, a thinking
part, and a doing
part:
-
thinking
: Three fundamental questions (see scissors header above), which can be addressed in any order.
Answering these three questions is an iterative process — the team moves back and forth between them as changes in thinking in one question or learning from PDSA cycles results in changes in thinking in another. doing
: The Rapid PDSA cycle
to test and adapt changes to ensure they result in the desired improvement.
1.Aim statement ( SMART Aim Statement)
A statement of the aim:
- Provides leaders a mechanism to think through all aspects of the proposed effort
-
Aids in selection of the team to make the improvements.
The members of the team should be selected from those who are knowledgeable about the processes or services that are likely to be studied, or who have a stake in their performance. - Reduces variation in activities from the original purpose
- Helps in the selection of particular processes or products for study
- Empowers individuals to make changes in health care systems
- Clarifies the magnitude of improvement expected from the project
- Defines the time frame for the improvement work.
Good aim statements are clear, concise, and results oriented. They should be aligned with the goals of the organization to clarify why the work is being done. Setting numerical targets helps focus measurements used in the improvement effort. Numerical goals can also be abused and lead to bad practices, so those providing a goal should convince the team that the goal is feasible by:
- Providing the level of support and resources that will be required to achieve the goals
- Observing other organizations that have made similar accomplishments
- Providing some basic ideas that could feasibl result in achieving the goals
- Demonstrating the benefit to the organization if the goals could be achieved.
2.Measures
Project teams use measures to give them feedback that the changes they are making
are having the desired impact.
Some measures should focus at the project level (global measures) and
be maintained throughout the project. Other measures are done on an as-needed basis
as part of PDSA Cycles for assessment of the changes tested. The Cycle measures
would include interviews with staff and patients affected by tests, and more
specific time measures to understand cycle efficiency.
Because improvements are made over time, measures should be displayed on run charts or Shewhart control charts. The time-ordered charts of a set of global measures will provide the primary way to assess the impact of each project team's work. Rather than just doing a before-and-after assessment, feedback from the measures is consistent and ongoing throughout the project. This approach gives teams the opportunity to work on data collection problems and to communicate their progress every month of the project. Key changes made to care systems can be annotated on the charts to give an analysis of the impact of the changes.
3.Changes
Developing a change that will help accomplish the project aim usually requires making a fundamental change to the system. There are two types of change:
- Changes that are needed to keep the system performing at current levels (first-order change)
- Changes that are needed to improve the system or create a new system (second-order change)
The important notion is not the size of the change but the impact of the change. Big improvements can often be realized by making small changes directed at the right places in the system. Most improvement efforts require second-order changes because they:
- Require design or redesign of some aspect of the system
- Are necessary for improving a system that does not have many problems
- Fundamentally alter how the system works and what people do in the system
- Often result in improvement of several measures simultaneously
- Require design or redesign of some aspect of the system
Second-order changes can be developed by critical thinking about the current system, learning from approaches in other organizations, using new technology, applying creative thinking methods, or by using concepts that have worked in other improvement situations.
- Outcome
- Process
- Balancing
Any single measure is probably inadequate to support a system improvement. But when
the measures are taken together, as a small family, they are powerful. .
Measures help teams answer the second question of the Model for Improvement.
Use feedback in the form of quantitative and qualitative data to learn
if a specific change leads to an improvement. .
Ensure that the individuals who will most benefit from the improvement
contribute to identifying measures that reflect improvement from their perspective.
Almost all improvement activities should include one or more outcome measures.
Process measures are useful because they are logically connected to the outcome measure(s) and typically show improvement before the outcome measure does. They are early indicators of whether or not changes are improvements. It is easy to overdo measurement, especially process measures. Collecting data for too many measures can reduce the time available for testing changes.
Balancing measures aid in detecting unintended consequences. For example,
a decrease in the length of stay (LOS) of patients in ICU may be accompanied by an
increase in the patient returns to ICU rate.
A balancing measure also aids in tracking events that would provide a rival explanation
for an improvement. In this example if the goal is to reduce the ICU LOS, it may be
useful to measure the volume of workload to see if it, rather than the changes that you made,
explains any improvement in the LOS.
| Type of Measure | Indicators |
|---|---|
| Outcome | • Surgical Site Infection (SSI) rate |
| Process |
• Percentage of appropriate prophylactic antibiotic selection • Percentage of on-time administration of prophylactic antibiotics • Percentage of staff with a safety culture climate score greater than 4 |
| Balancing |
• Percent satisfaction • Cost per case |
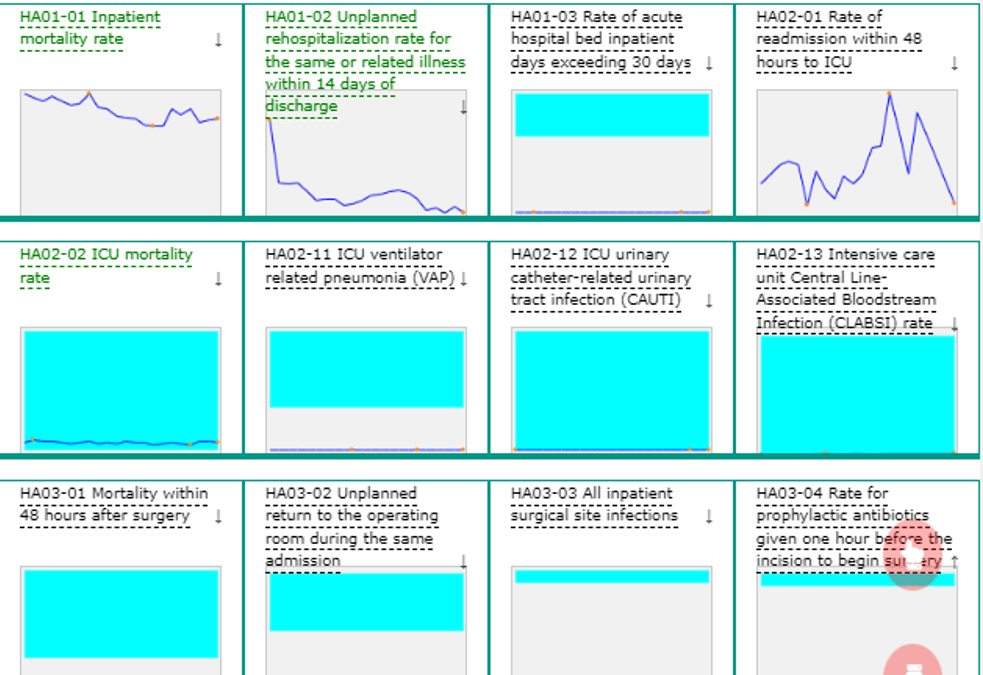
Family of Measures Dashboard
The usefulness of the family of measures is increased when they are viewed as a time
series (run charts, shewhart control charts) and presented all on one page (a dashboard
).
Figure 1 shows an indicator package displayed graphically all on the same page.
This allows visualizing the impact changes are having on the system, rather than on just a single measure.
References
- Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. www.ihi.org/resources/publications/ (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
- GreenDot Consulting Group. SMART Aim statement. www.thegreendotgroup.com/
- Provost LP, Murray SK. The Health Care Data Guide: Learning from Data for Improvement www.amazon.com/